Laparoscopic surgery, also known as keyhole surgery, is a minimally invasive surgery technique. It allows access to the abdomen without large incisions in the skin. Laparoscopic procedures can be used both for the diagnosis and treatment of patients, with over 13 million laparoscopic procedures taking place every year1.
Low Impact
Laparoscopy
When compared to open surgery, laparoscopic surgery provides benefits such as faster patient recovery and reduced surgical risk. It can also become a more cost-effective solution for hospitals without compromising patient safety2. Despite this, the invasiveness of laparoscopic surgery could still be reduced even further.
Although less invasive than open surgery, normal laparoscopy is still associated with high use of analgesics (painkillers), with a study finding that there was no difference in pain medication for minor or major surgery3. To reduce postoperative pain and consequently speed up patient discharge, low impact laparoscopy is designed to keep the patient as close to their natural state as possible during procedures.
Our concept of low impact laparoscopy is defined as a minimally invasive technique that combines low-pressure insufflation and microscopy, which would have the advantage of reducing postoperative pain to improve outpatient management. The innovative surgical protocol combines different surgical techniques and tools to minimise the invasiveness of surgery.
What is
low pressure laparoscopy
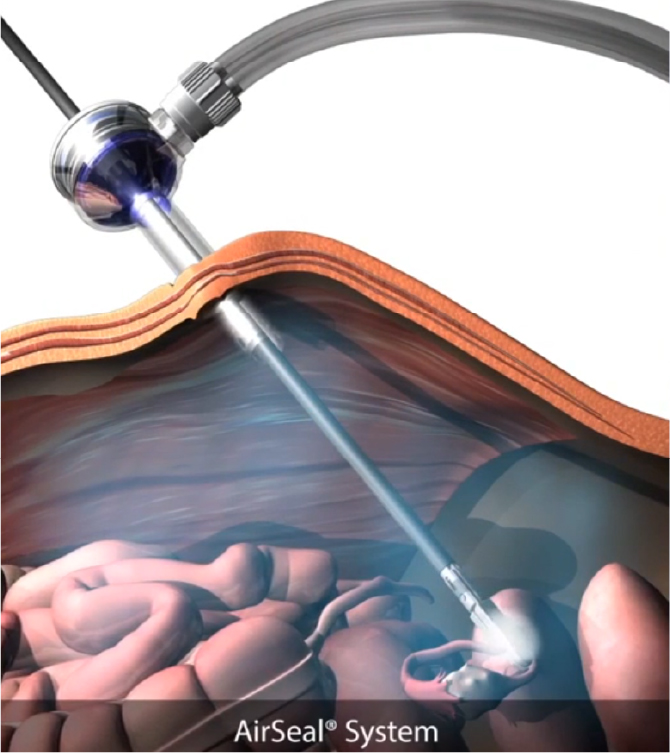
During laparoscopic surgery, the pneumoperitoneum is required to create a workspace between the abdominal wall and the intraabdominal organs. Traditionally, most General Surgeons will begin operating at 15 mmHg and then drop to around 12 mmHg. Other specialities, particularly Gynaecology, begin at much higher pressures and maintain those higher pressures. Unfortunately, increased intraabdominal pressure comes with side effects such as shoulder pain. It may also have a negative impact on cardiovascular, pulmonary and intraabdominal organ functioning4.
During low pressure laparoscopy, it is possible to reduce the pressure from what is perceived as the norm of 12 to between 6-8. The reduction in pressure leads to better patient outcomes, without needing to compromise surgical vision during the procedure5.
What are the impacts
of low-pressure laparoscopy?
As previously mentioned, despite being considerably less invasive than open surgery, laparoscopy can still result in postoperative pain. In fact, 80% of patients complain of high pain levels and require pain relief after laparoscopic surgery6.
This can be because of the retention of CO₂ in the abdomen, which can irritate the phrenic nerve leading to postoperative shoulder pain, which is one of the leading causes of patient discomfort and can last up to three days after surgery. Trapped CO₂ between the liver and right diaphragm can also cause abdominal pain7. In some instances, the complications of pain can lead to readmission.
In a study by Radosa et al. two groups were compared, 87 patients had 8 mmHg, and 19 had the standard 12 mmHg. Their postoperative symptoms were reviewed at 3, 24 and 48 hours to conclude that shoulder tip pain was lower in the low pressure group (p>0.001)8.
Due to having less postoperative pain and pressure, patients may be discharged earlier. A study published in 2014 found that almost half of patients (46.7%) operated on at low pressure considered discharge on the same day possible, compared to 23% of patients operated on at standard pressure (p=.058)⁹. A further study saw a 49% decrease in PACU time and a 64% decrease in length of stay with patients who had a low-pressure laparoscopic ventral hernia surgery¹⁰.
Postoperative ileus is a deceleration of the motility of bowel movement, more commonly known as bowel obstruction. It has been shown to lengthen hospital stays and increase hospital costs, in fact, the overall annual expenditure in the US secondary to postoperative ileus is around $750 million to $1 billion¹¹.
High-pressure pneumoperitoneum may cause systemic inflammation and affect the immune response in the early postoperative period. This inflammation can be a contributing factor to postoperative ileus.
In April 2017, Lawmed received 10,000 UK pounds funding from the East and North Hertfordshire NHS Trust to pilot the world’s first study looking into the impact of intra and postoperative cytokine levels in 20 patients undergoing a Trans Peritoneal Robotic Prostatectomy by a single surgeon.
Patients were divvied into 2 groups, one with higher pressure (15 mmHg) and the other with a low pressure (12 mmHg) using the AirSeal® insufflation system. The incidence of ileus was higher at a pressure of 15 mmHg – 2/10(20%) as against a pressure of 12 mmHg (0/10)¹².
THE DIFFERENCE BETWEEN LOW PRESSURE AND LOW IMPACT LAPAROSCOPY
Low pressure laparoscopy on its own is more widely practiced than full low impact laparoscopy protocol, but there needs to be a shift to begin improving laparoscopy much more broadly. Low pressure laparoscopy is just the beginning.
Low impact laparoscopy looks to impact the whole procedure, not just the pressure element. It aims to keep the patient’s anatomy as close to its natural state as possible, making minimal changes with the aim of improving recovery.
WHY IS THERE A NEED
FOR LOW IMPACT SURGERY?
GUIDELINES
Many associations and societies have recommended that by reducing the impact of surgery we can increase the possibilities of better patient outcomes.
The European Association of Endoscopic Surgeons (EAES) guidelines state that when operating laparoscopically, the lowest possible pressure level should be applied and the lowest diameter instruments and evacuate the gas at the end of the procedure.
In addition, there was a requirement to remove residual gas. These are the definitions described by EAES:
- Apply lowest possible pressure level (Grade A)
- Use small instruments, if suitable (Grade A)
- At the end of the operation, remove residual gas (Grade B)
STREAMLINING THE PATIENT
PATHWAY
The NHS has been under pressure to shorten waiting lists for years, but the onset of the Covid-19 pandemic and the disruption to elective treatment has meant that waiting lists have reached their highest ever levels.
More than ever, patient pathways need to be streamlined, to treat patients more efficiently and reduce hospital stays.
Amongst other factors, low impact surgery may result in less pain for patients allowing them to recover faster. This can result to reduced PACU time and quicker discharge, without compromising patient safety.
HOW CAN LOW IMPACT
LAPAROSCOPY BE ACHIEVED?
There are other ways, beyond low pressure that make a surgery low impact. Low pressure is of course a strong factor, but other factors include the creation of smaller incisions.
Low impact laparoscopy can see incisions reduced to 3 mm from 5-10 mm by using 3 mm instruments and ports, this is sometimes known as microlaparoscopy. There are many different reasons why this might be beneficial to patients and hospitals.
Shorter hospital stays
Patients treated through microlaparoscopy may be able to leave hospital sooner. A 2009 study found that hospital stays were brought down from an average of 3 days to 2 days for patients with smaller incisions¹³.
Reduces pain
In a double-blind controlled study, 60 patients were randomized to undergo either microlaparoscopic cholecystectomy using one 10-mm and three 3.5-mm trocars or traditional laparoscopic cholecystectomy using two 10-mm and two 5-mm trocars. In the 3.5-mm LC group, incisional pain was significantly decreased in the 1st postoperative week as compared with the LC group (p <0.01)¹⁴.
Improves cosmesis
Smaller incisions improve the cosmetic preservation of the patient.
Staff do not need to be retained
Typically, advantages in surgery come with a learning curve; however, low impact laparoscopy operates in the same way as normal laparoscopy. Therefore, there is no need to spend valuable time retraining staff. In addition, with the advent of newer, stronger, 3 mm instruments, such as EvoLap, there is an ability to manipulate heavier organs and tissues.
USING LOW IMPACT AS
PROTOCOL
All of the techniques that have been discussed can lower the impact of surgery, however, for optimal results they should be used in conjunction for a low-impact laparoscopy surgical protocol.

There are many successful examples of using a low impact approach; for more details see the bibliography below.
We believe low-impact laparoscopy is the next step in laparoscopic surgery in order to reduce patient pain, and recovery time and speed up patient discharge with the result of greater patient throughput in surgery.
References
1. https://idataresearch.com/over-13-million-laparoscopic-procedures-are-performed-globally-every-year/
2. Buia, Alexander et al. “Laparoscopic surgery: A qualified systematic review.” World journal of methodology vol. 5,4 238-54. 26 Dec. 2015, doi:10.5662/wjm.v5.i4.238.
3. Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, Bohnert ASB, Kheterpal S, Nallamothu BK. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017 Jun 21;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. Epub 2017 Jun 21. Erratum in: JAMA Surg. 2019 Mar 1;154(3):272. PMID: 28403427; PMCID: PMC7050825.
4. Özdemir-van Brunschot, D.M.D., van Laarhoven, K.C.J.H.M., Scheffer, GJ. et al. What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg Endosc 30, 2049–2065 (2016). https://doi.org/10.1007/s00464-015-4454-9.
5. Bogani G, Uccella S, Cromi A, Serati M, Casarin J, Pinelli C, Ghezzi F. Low vs standard pneumoperitoneum pressure during laparoscopic hysterectomy: prospective randomized trial. J Minim Invasive Gynecol. 2014 May-Jun;21(3):466-71. doi: 10.1016/j.jmig.2013.12.091. Epub 2013 Dec 25. PMID: 24374246.
6. Sao CH, Chan-Tiopianco M, Chung KC, Chen YJ, Horng HC, Lee WL, Wang PH. Pain after laparoscopic surgery: Focus on shoulder-tip pain after gynecological laparoscopic surgery. J Chin Med Assoc. 2019 Nov;82(11):819-826. doi: 10.1097/JCMA.0000000000000190. PMID: 31517775.
7.Tsai H, Chen Y, Ho C, et al. Maneuvers to Decrease Laparoscopy-Induced Shoulder and Upper Abdominal Pain: A Randomized Controlled Study. Arch Surg. 2011;146(12):1360–1366. doi:10.1001/archsurg.2011.597.
8. Radosa, JC, Radosa, MP, Schweitzer, PA, Radosa, CG, Stotz, L, Hamza, A, Takacs, Z, Lepper, PM, Wagenpfeil, S, Linxweiler, M, Morinello, E, Solomayer, E-F. Impact of different intraoperative CO2 pressure levels (8 and 15 mmHg) during laparoscopic hysterectomy performed due to benign uterine pathologies on postoperative pain and arterial pCO2: a prospective randomised controlled clinical trial. BJOG 2019; 126: 1276– 1285.
9. Laparoscopic Surgery at Low Pressure (7 mmHg) with AirSeal® System; a Comparative Prospective Pilot Study with a Standard Insufflation (15 mmHg) in 60 Patients.
10. Low Impact Laparoscopic Ventral Hernia Surgery using AirSeal® System https://static1.squarespace.com/static/5e470053aa4b8d210899d1ba/t/5ec6cf707ee48b49e8e47967/1590087538614/SurgiQuest+Whitepaper.pdf
11.https://teachmesurgery.com/perioperative/gastrointestinal/ileus/.
12.Rohloff M, Cicic A, Christensen C, Maatman TK, Lindberg J, Maatman TJ. Reduction in postoperative ileus rates utilizing lower pressure pneumoperitoneum in robotic-assisted radical prostatectomy. J Robot Surg. 2019 Oct;13(5):671-674. doi: 10.1007/s11701-018-00915-w. Epub 2019 Jan 2. PMID: 30604275.
13. Ghezzi F, Cromi A, Siesto G, Zefiro F, Franchi M, Bolis P. Microlaparoscopy: a further development of minimally invasive surgery for endometrial cancer staging — initial experience. Gynecol Oncol. 2009 May;113(2):170-5. doi: 10.1016/j.ygyno.2009.01.015. Epub 2009 Feb 24. PMID: 19243814.
14. https://link.springer.com/article/10.1007/s00464-001-9026-5
15. Yeung PP Jr, Bolden CR, Westreich D, Sobolewski C. Patient preferences of cosmesis for abdominal incisions in gynecologic surgery. J Minim Invasive Gynecol. 2013 Jan-Feb;20(1):79-84. doi: 10.1016/j.jmig.2012.09.008. PMID: 23312246.